Q. What happens if the secondary payment is posted before the primary?
A. The payment will still post properly. The responsible party will not change unless the service line balance is zero at which point the responsible party will be set to 'Patient.'
Q. What happens if an 835 file is posted twice?
A. No new payment will be created and no new disbursements will be created since all of them will find 'matching' disbursements. If you select adjustments to apply, they will either find a matching adjustment or the adjustment will be applied. If you apply adjustments that were previously tracked, the tracking adjustment will be removed and the adjustment will be applied.
Q. What happens if an 835 is posted for a payment that was manually entered with the same reference number?
A. No new payment will be created and no new disbursements will be created since all of them will find 'matching' disbursements. If you select adjustments to apply, they may be applied if there is no matching reference number.
Q. What happens if an 835 is posted for a payment that was manually entered with a different reference number?
A. The program will create a payment based on the 835 data. The program will post disbursements from the 835 since there are no 'matching' disbursements. If the option to over pay is turned on, the claim will have a credit balance, otherwise posting may cause a 'BALANCE EXCEEDED' message.
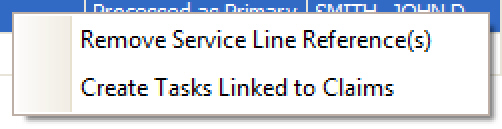
Q. How do I prevent a service line from having payments or adjustments applied?
A. Remove the service line reference by right clicking the service line(s) and select ‘Remove Service Line Reference(s)’.
Q. How does the program match the payment data to the service lines?
A. When Premier sends an 837 file to the payer, there is a special ID number that is assigned to each service line (REF*6R for you ANSI junkies). This special ID number comes back in the 835 ERA and Premier uses it to match back to the service line. If the special ID does not exist in the 835, EZClaim falls to its secondary matches which look at the CLP01 field to try and match the claim based on the claim’s invoice number or Claim ID along with the patient’s first and last name. Premier then looks at the procedure code, charge, and service date. If needed, it will also include modifiers in the match.
Q. Why does the program separate out Provider Level Adjustments rather than processing them within an 835 ERA file?
A. When payers return Provider Level Adjustment (also called PLA or PLB) information within an 835 file, very often they do not provide the claim level (or service line level) detail the program needs in order to complete the auto posting “loop” and post the payments and/or adjustments accurately. For example, during the review process, the payer may determine that they owe you interest, or that you have been overpaid and thus they are adjusting payments, in order to balance your account. We suggest contacting the payer directly to see if you can obtain patient/claim/service specific data you can then post manually within your Premier program. Once you have printed the Provider Level Adjustment information out for further determination as needed, you can then proceed to auto post the rest of the data contained in the 835.
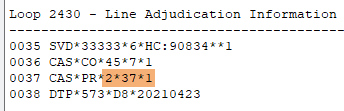
Q. What if my payer requires “unbundled” PR adjustments?
Solution
•Added a payer option to 'Unbundle PR adjustments exported in Loop 2430'
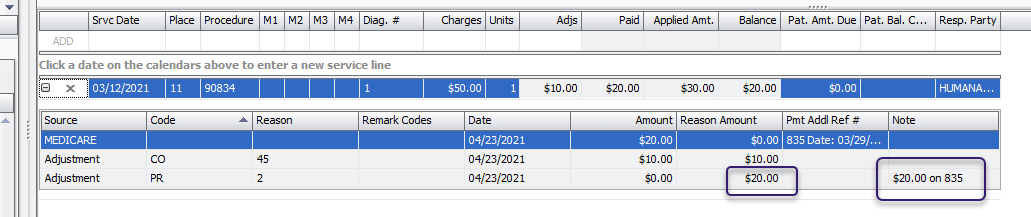
•Added a new service line level column called 'Reason Amount'
o Used to report dollar amount assigned by payer to each Reason code
o Does not affect service line balance
How to Use with Auto Posting
•The Reason Amount is automatically filled according to what is in the 835 data. It’s the same data used to populate the Note field.
•The tracked PR Reason Amounts must equal the service line balance in order to unbundle. If not, Premier will continue to bundle them into a single PR2.
•Reason Amounts on CO, OA, and other adjustments are not affected.
•Bill-To Payer must have the unbundled option checked at the Payer Library level. (See screenshot below.)
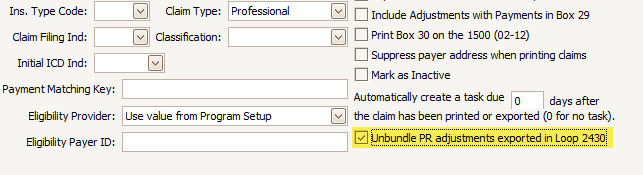
UNBUNDLED secondary 837 generation
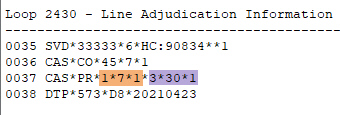
BUNDLED secondary 837 generation for comparison