

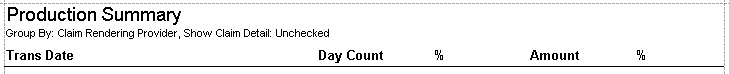
Shows the production breakdown of Charges, Adjustments and Disbursements. Displays the percent of total for each grouping. To customize your report, enter data into the ‘Report Criteria’ fields.
The Day Count represents the number of unique dates. Therefore, if running the report by Rendering provider, the Day Count in the ‘Charges’ section would represent the number of days the provider was in the office performing services. The number is not very relevant in the other sections.
The Day Count counts the unique dates over the group. This means the total Day Count may be less than the total of each group. If Doctor A saw patients on 10/1 and 10/2, the Day Count would be 2. If Doctor B saw patients on 10/1 and 10/3, the Day Count would be 2. The total Day Count will be 3 (not 4) since patients were seen on 10/1, 10/2, and 10/3.
Transactions shown on the report
•Charges - Trans Date = From Date
•Contract Adjustments - Trans Date = Adjustment Date
•Disbursements - Trans Date = Payment Date. Disbursements are used instead of payments because the report can be grouped by claim related data and payments are not linked to claims until disbursed.
•Other Adjustments - Trans Date = Adjustment Date