Before submitting your secondary claims, confirm the following or errors may be generated.
Payer Library (Step 1)
•In the Payer Library, if the Secondary payer is Medicare, confirm that Medicare secondary ‘Ins.Type Code’ is selected.
Patient Information screen (Step 2)
•Secondary Insured’s Name, DOB and Gender are entered.
•If Medicare/Medicaid Other Insured Policy or Group number field is blank.
•Secondary (and Primary) Insurance with Payer ID is entered.
•SSN, Patient Member ID and Additional ID number are blank. See Additional Information.
•Secondary/Other Insured’s ID# is entered in the ‘Insured’s ID’ field.
•Secondary subscriber ‘Patient Rel to Insured’ is selected.
Claim screen (Step 3)
•Confirm Payment information entered matches the EOB.
•Confirm each service line has an Insurance payment entered even if it is a $0.00.
•Line Item payments and/or adjustments with a date have been entered.
•Confirm ‘Bill To:’ has been set to ‘Secondary Insurance’.
•In the ‘Claim Grid’ confirm the ‘Ignore Applied Amount’ box is unchecked.
Your claim is now ready for submission or printing.
2320 COB CLAIM BALANCING FAILED. (Balancing error) Step 3
•All service lines did not have payment entered and/or payment amounts were incorrect.
OTHER SUBSCRIBER INFORMATION IS MISSING OR INVALID
•Patient Information screen – Confirm ‘Secondary Insured’s’ information is entered. Step 2
•Patient Information – Confirm BOTH insurances have a Payer ID. Step 1. Also make sure the ‘Insured’s ID’ field has the secondary ID. Step 2
OTHER PAYER SUBSCRIBER PRIMARY IDENTIFICATION NUMBER IS MISSING OR INVALID
•Patient Information screen – Confirm ‘Secondary Insured’s ID’ field has secondary subscriber ID entered. Step 2
•Patient Information screen – Confirm ‘Insured’s Policy or Group’ number field is blank. Step 2
INSURANCE TYPE CODE MISSING OR INVALID
•Payer Library – In the ‘Insurance Type’ drop-down box choose one of the numbers for Medicare secondary Insurance ‘Type Code’. Step 1
INSURANCE TYPE CODE IS MISSING OR INVALID. (Bad Data: MB)
•Payer Library – Usually this is for a Medicare claim when MB is indicated as the bad data. In the ‘Ins Type’ drop-down box choose one of the numbers for ‘Medicare Secondary Claims’. Step 1
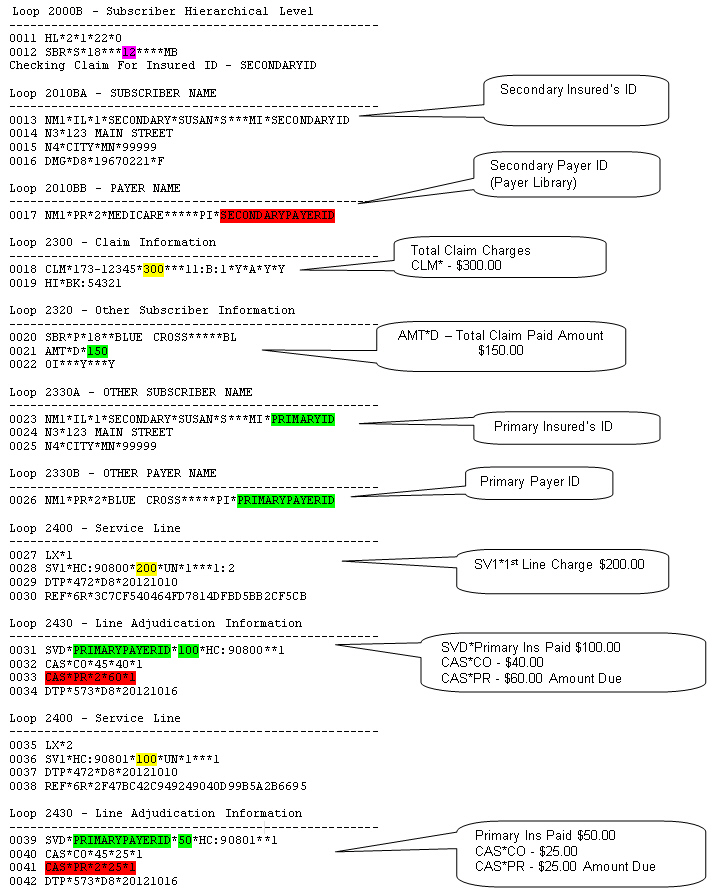
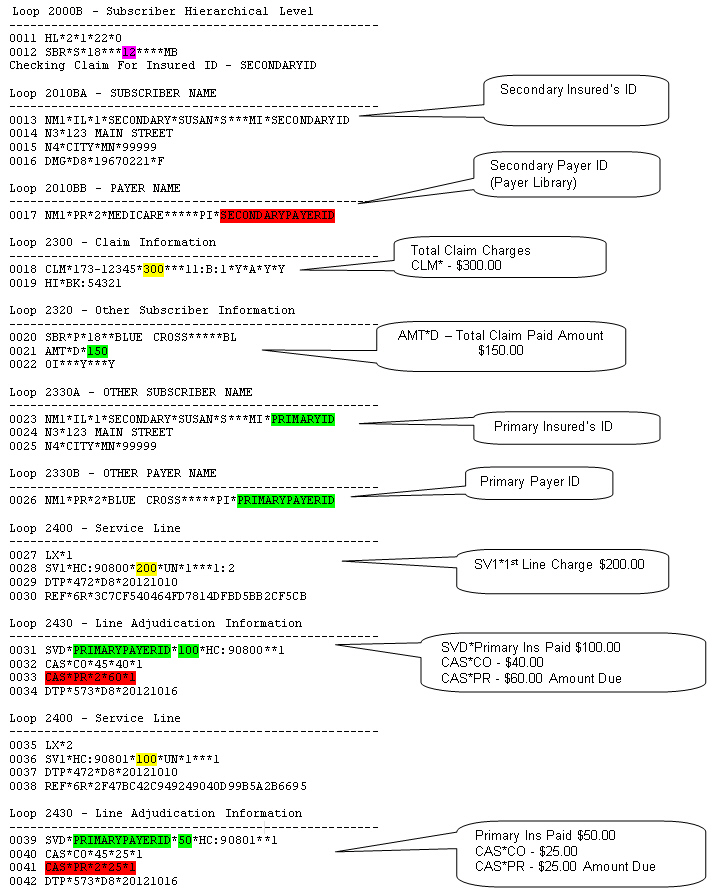
Use this sample of an analyzed Secondary claim to confirm data. See sample below.
How to Analyze a Claim
1. Go to ‘Electronic Billing’.
2. Select ‘Send Claims’.
3. Select by checking the claim to be analyzed.
4. Use the Check for Errors drop-down box and choose ‘Detailed Report’.
5. Compare to sample below. (Sample is for a Medicare secondary claim your claim may include different data depending on your payer.)