 button to drill down to view warning
status.
button to drill down to view warning
status.Click on the ‘Apply Payment and Adjustments’ button.
Confirm line item information is green. If not, click on the  button to drill down to view warning
status.
button to drill down to view warning
status.
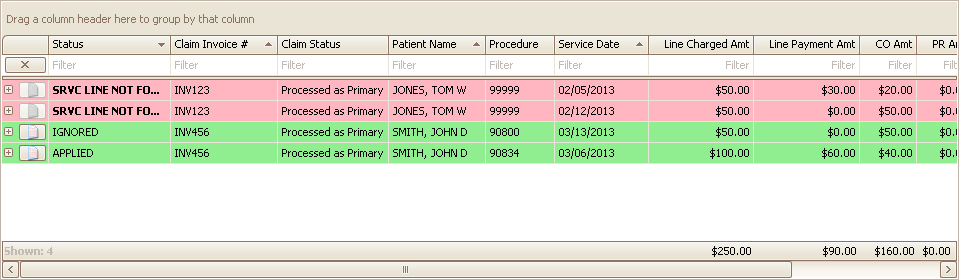
After the program has applied payments and adjustments, the Options grid will reflect the status of each Payment and Adjustment;
•MATCHED (Green): The payment or adjustment already exists.
•APPLIED (Green): The payment or adjustment dollar amount was applied.
•TRACKED (Green): The payment or adjustment was entered with a $0.00-dollar amount.
•IGNORED (Green): The payment or adjustment was not entered.
•WARNING (Yellow): One of the adjustments for the service line have an issue. Click the + sign to drill down to the adjustment issue.
•MISMATCH (Red): The program found an existing value but it does not match the incoming 835 data.
•SRVC LINE NOT FOUND (Red): Service Line ID returned in the 835 (REF*6R) is invalid or missing.
•BALANCED EXCEEDED (Red): Posting the payment or adjustment would have caused the balance to go negative. If you actually want this to happen (due to a double or overpayment), you can change the 835 option. See Posting Options for more information.
Claim payments with an ‘835 status code of 22’ (Reversal of Previous Payment) will be posted unless the option not to post them is turned on. See Posting Options for more information on posting options.
Claim payments with an ‘835 status code of 4’ (Denied) are not posted. The claim posting status will be flagged as ‘PROCESSED’ but the payment posting status will be set to ‘IGNORED.’
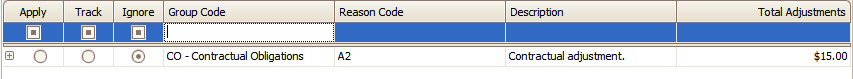
Any adjustments from claims with a ‘status of 4’ will be listed on the adjustment posting grid so they can be tracked for follow-up purposes.
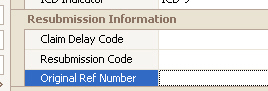
Keywords: Orig Ref No, Original Ref No, ORN
The original reference number found in segment CLP07 (Payer Claim Control Number) of the 835 will populate the claim field ‘Original Ref Number’ if the field is currently blank. This facilitates secondary billing with some payers who require a reference number or for claim resubmission.
Enter only if required by your Payer.
Even when a payer requests a “corrected” claim, using 6 as the Resubmission Code will likely cause claim rejections at the clearinghouse level. (The 6 does not seem to cause issues in certain billing situations, thus Premier still makes it available in the drop-down.) We suggest using Resub Code 7 instead.
Also, the Original Ref Number is required so that the payer can identify what claim is being replaced in their processing system. You can obtain this number as follows:
1. The program auto-populates the Original Ref Number during ERA auto-posting.
2. The Original Ref No may be available on a payer report. It is sometimes called an ICN, Internal Control Number, etc.
3. You may need to contact the payer directly to obtain the Original Ref Number it is not otherwise available to you.
When auto posting 835 data, the program uses the claim status returned in the CLP segment to determine if a claim should be marked as ‘Ready to Submit’ or ‘Submitted.’
The 835-claim status codes may be one of the following:
1 = Processed as Primary
2 = Processed as Secondary
3 = Processed as Tertiary
19 = Processed as Primary, Forwarded to Additional Payer(s)
20 = Processed as Secondary, Forwarded to Additional Payer(s)
21 = Processed as Tertiary, Forwarded to Additional Payer(s)
If the claim has additional payers AND the 835-claim status is 1, 2, or 3, the program will change the ‘Bill To’ to the next payer in line and mark the claim as ‘Ready to Submit’
If the claim has additional payers AND the 835-claim status is 19, 20, or 21, the program will change the ‘Bill To’ to the next payer in line and mark the claim as ‘Submitted’