EZClaim cannot answer questions about the use of ICD-10 codes. Please contact your payer for any questions related to the use of ICD-10 codes. This section points out features of EZClaim Premier that relate to the ICD indicator. This indicator is used to determine if the diagnosis codes should be treated as ICD-9 or ICD-10 codes by the payer.
CMS Web Site on ICD-10: http://www.cms.gov/icd10
You cannot mix ICD-9 and ICD-10 codes on one claim.
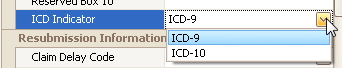
Claim ICD Indicator
The claim screen has an ICD indicator field located in the ‘Misc Information’ section of the grid. The field has two options; ICD-9 and ICD-10.
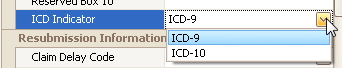
Initial Value
The program will automatically set the ICD Indicator to the value selected in program setup. See “Program Setup” > Claim for information on changing the value.
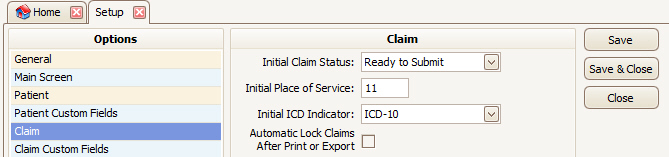
Code Library
There are two code libraries available for diagnosis codes. Use ‘Diagnosis Codes’ for ICD-9 and ‘Diagnosis Codes ICD-10’ for ICD-10 codes. See Code Library for information on the code libraries.
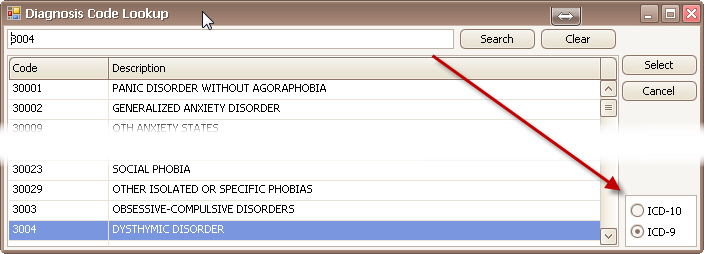
Diagnosis Code Library Lookup
When using the code library to look up a diagnosis code, a filter option is available. To look up a diagnosis code, double click in the diagnosis field.
Paper Claims
The ICD Indicator prints in Box 21 on the CMS-1500 form. The valid values are ‘9’ for ICD-9 or ‘0’ for ICD-10.
Electronic Claims
The ICD Indicator will affect the Code List Qualifier Code used in HI segments in Loop 2300. When ICD-10 is the indicator value, the qualifiers are prefixed with an ‘A’.
ICD-9 example: HI*BK:11111*BF:22222
ICD-10 example: HK*ABK:33333*ABF:44444