Home tab >
Payer Library
Home tab >
Payer Library Home tab >
Payer Library
Home tab >
Payer Library
The ‘Payer Library’ is used to maintain Payer information and customize Payer options.
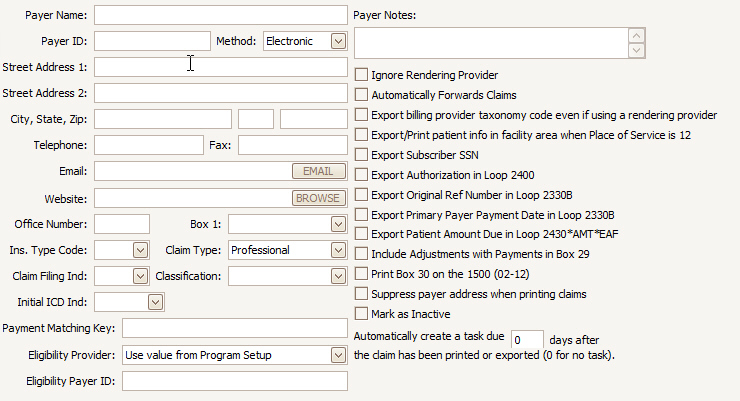
Payer Library Fields:
•Payer Name and Address information.
•Payer ID – The code provided by the payer or clearinghouse to designate this payer. For electronic billing, the Payer ID is required. Especially if you have multiple entries for the same payer (such as UHC having different mailing addresses, etc.) this is critical in making the payment posting work smoothly. The program uses the Payer ID to link multiple payer library entries together when posting payments. Payment Matching Key may also be useful in these situations. Please see below for more information.
•Method – Select the method of transmission, Paper or Electronic.
•Ins. Type Code - Insurance Type Code is used when submitting Medicare Secondary Payer electronic claims. Note: there is an “Insurance Type Code Override” field on the claim grid if you need to override the value in the payer library. This eliminates the need for duplicate payer library entries for the sole purpose of a different insurance type code.
•Claim Filing Indicator – A code identifying the source or type of payment for the claim.
•Classification – Often, for reporting and grouping purposes, it’s easier to use a classification instead of the payer name. For example, you may have multiple Blue Cross entries created for different billing scenarios. Setting the Classification to ‘BCBS’ would help run reports on all the Blue Cross entries without having to select each entry individually. Note that the payer classification criteria are only available on certain reports.
•Initial ICD Ind – This is used for setting the ICD indicator on new claims that use this payer. This setting overrides the ICD indicator setting in Program Setup.
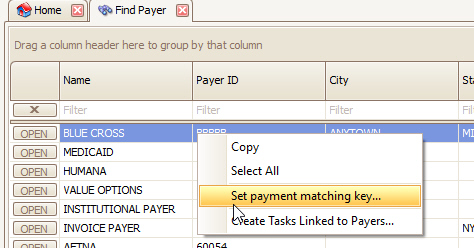
•Payment Matching Key - This field may be used to make the program consider multiple payers equivalent to each other from a posting / payment entry perspective. For example, a user may enter ‘Blue’ for each of their Blue Cross, Blue Shield, etc., and all payers with ‘Blue’ in that field will be treated as if they were the same payer for auto-posting purposes. Payment Matching Key may be updated in bulk at the ‘Find Payer’ window by right clicking the payers you wish to edit.
•Eligibility Payer ID – This is used for situations where the Payer ID for eligibility verification is different from the payer ID for claims submission.
Payer Library Options
•Ignore Rendering Provider – Ignores the Rendering Provider information when claim is printed or exported.
•Automatically Forwards Claims – Certain payers (notably Medicare) forward claims to the secondary and/or tertiary payer. When checked, claims that switch from primary to secondary will be marked as ‘Submitted’ so they are not printed or exported by the user, since they have automatically been forwarded. IMPORTANT: When auto-posting, the Claim Status reported in the 835 determines whether the secondary (or tertiary) claim will be set to ‘Ready to Submit’ or ‘Submitted’. Example: If the 835 says the claim was ‘Processed as Primary, Forwarded to Additional Payer(s)’ then the status of the secondary claim will be set to ‘Submitted’. If the 835 says the claim was ‘Processed as Primary’ then the status of the secondary claim will be set to ‘Ready to Submit’.
•Export billing provider taxonomy code even if using a rendering provider – Check this box to export billing provider taxonomy in Loop 2000A Segment PRV Field 02 even if a rendering provider is selected on a claim.
•Export/Print patient info in Facility loop when Place of service is 12 – Primarily used by Home Health providers.
•Export Subscriber SSN – Check this box if the payer requires the subscriber SSN in the ANSI 837 file. Must be entered on Primary or Secondary Ins tab in the ‘Subscriber SSN’ field.
•Export Authorization in Loop 2400 – Check this box to export the authorization in loop 2400 instead of the standard loop 2300.
•Export Original Ref Number in Loop 2330B – Check this box to export the original ref number in loop 2330B.
•Export Primary Payer Payment Date in Loop 2330B – Check this box when the payer requires this info on secondary claims.
•Export Patient Amount Due in Loop 2430*AMT*EAF – Check this box when the payer requires this info on secondary claims.
•Include Adjustments with Payments in Box 29 – When checked, the amount printed in Box 29 will include adjustments.
•Print Box 30 on the 1500 (02-12) – Check this box to print the balance due in box 30 for the 02-12 version of the 1500 form. This box is normally left blank.
•Suppress payer address when printing claims – Check this box to prevent the payer address from printing at the top of the 1500 form.
•Mark as Inactive – Check to prevent the Payer from being displayed in the Payer List.
•Automatically create a reminder task – Use this feature to have the system automatically create a task with a due date for X number of days after the claim has been billed. When a claim has been printed or exported, a task will be created with a due date for X number of days after the claim has been billed.
•Eligibility Provider – Use this field if needed to override the provider selected under the program setup option.
•Eligibility Payer ID – Use when the eligibility payer ID is different from the one used for claim submission.
See Payer Library for additional information on setting up the Payer Library.
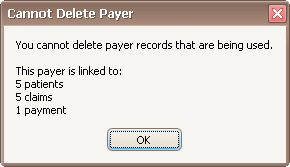
You cannot delete a payer entry if it is currently in use. If you try to delete an entry and it is currently being used, a message will appear showing where the entry is used. Use the Find tools to open the appropriate record and change payer selected. If the entry is being used and you no longer want it to show up in selection lists, mark the entry as inactive instead.