The workflow for payer rejections (post-adjudicated) is slightly different since the information is coming from a different source.
The following steps will take you through processing an ANSI 835 report and creating tasks for the rejected claims.
See Auto Posting Payments for information on auto posting payments.
1.
Click the View EDI Reports button.
2.
Download any new EDI reports.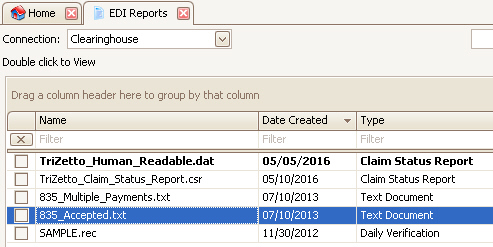
3. Double click the ANSI 835 report.
4.
Confirm the selected payer and click OK.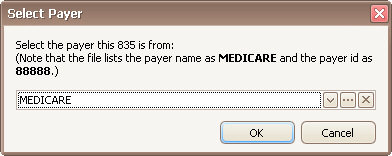
5.
At the bottom of the screen are all the reason codes. This reason code
indicates claims were rejected because the procedure code was invalid on the
date of service. These claims need to be fixed and resubmitted.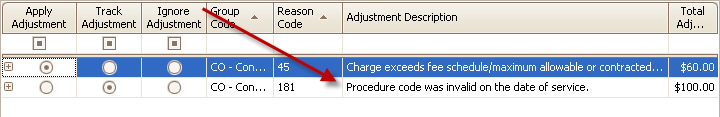
6.
Right click the reason code and select ‘Create Tasks Linked to Claims’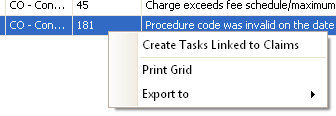
7.
Fill in the task information and click OK.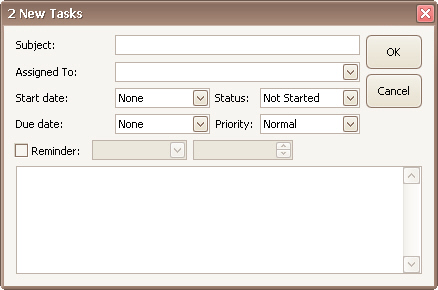
8.
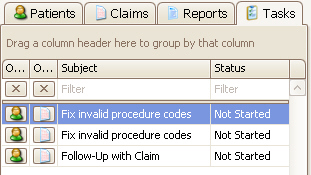
Use the Task list to open and work your rejected claims.